Long Non-Coding RNAs Emerging as Potential Epigenetic Biomarkers for Tobacco and/or Alcohol-Induced Head and Neck Cancer
Abstract
Head and Neck cancer (HNC) is one of the most prevalent and lethal cancer globally. The incidence of tobacco-induced HNC is gradually increasing in low and middle income countries. Among the various causative factors associated with HNCs, tobacco and alcohol play synergistic effect and are frequently associated with the risk of HNC. Tobacco-induced HNCs show distinct genetic and epigenetic alterations leading to different clinical outcomes in comparison to HPV-infected HNCs. Tobacco-induced HNCs are often associated with tumor aggressiveness, poor prognosis and low or nil prevalence of HPV infection. Apart from carcinogenic effects of these causative factors (use of tobacco products, alcohol intake and HPV or EBV infections), recent studies show that exposure to these factors alter/disrupt the regulation of non-coding RNAs including the long non-coding RNAs (lncRNAs). Altered lncRNA regulation is brought about by signalling networks that regulate cellular differentiation, apoptosis, angiogenesis and inflammatory pathways which play key functions in the genesis of different cancers including HNCs. There are numbers of studies supporting the emerging role of lncRNAs in development of HNC; however, reports connecting lncRNAs expression and addiction habits in HNC are still preliminary and sparse. Therefore, identification and characterization of lncRNAs that are differentially expressed upon exposure to risk-factors can serve as unique therapeutic targets and potential biomarker(s) for effective treatment of HNC subtypes. In this short review, we briefly reviewed the emerging role of lncRNAs in tobacco and alcohol induced HNCs.
Author Contributions
Academic Editor: Anil Tombak, Mersin University Medical Faculty, Turkey.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Shilpi Gupta, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Background
Head and neck cancer (HNC) represents a major public health problem globally. The incidence of tobacco-related HNC is increasing in low and middle income countries. Worldwide, HNCs accounts for ~80,7051 new cases and ~41,8323 deaths in 2018 1. HNCs originate from the upper head and neck region, including the lip, oral cavity, oropharynx, hypopharynx, nasopharynx, and larynx etc. Majority (≥90%) of HNCs result from chewing tobacco, smoking cigarette/bidi as well as due to alcohol intake 2, 3. Chewing Tobacco along-with betel, areca nut and slaked lime is more common in India and Asian countries. Tobacco smoke exerts inflammatory and suppressive effects on immune cells, alters mucosal immunity and promotes autoimmunity, resulting in HNCs. In the last few years, high-risk-human papillomaviruses (HR-HPVs) infection has become an independent risk factor for HNCs. HR-HPV infected HNCs show high variability across populations and geographic regions, mainly in Asian countries where the use of tobacco products is a regular part of the social life and tradition. Tobacco-induced HNCs show distinct genetic, epigenetic alterations, which can often be correlated with clinical outcome of HNC patients than HPV-infected HNCs. Tobacco-associated HNCs are often associated with aggressive metastasis, worst prognosis and low or nil of HPV prevalence. Association of different life style factors with HNC leads to heterogeneities and genetic/epigenetic changes. These genetic and epigenetic variations further effect outcome of the disease.
Even with the advances in the diagnosis and treatment methods, the 5-year survival (45%-50%) of HNC patients has not improved significantly over the last decade 4. Therefore, prevention of postoperative recurrence and improvement of patient survival poses a major challenge in HNC diagnosis and treatment. To date, there is no significant potential molecular marker for development of effective targeted molecular therapies to treat HNC patients 5. It seems, it is essential to investigate and identify therapeutic biomarkers based on risk-factors association for HNC patients. A number reports have illustrated that numerous non-coding RNAs (ncRNAs) can act as oncogenes and tumor suppressor genes playing key regulatory roles in the disease development and pathophysiology of various cancers. In the several dysregulated ncRNAs in HNCs, long noncoding RNAs (lncRNAs) (>200-nts in length) are a focus of current research providing suitable approaches for clinical treatment of HNCs. Recent evidences discovered that the lncRNAs can also serve as therapeutic targets at transcriptional, post-transcriptional and epigenetic levels 6, 7.
Tobacco and / or Alcohol Associated Head and Neck Cancers
Tobacco smoking and alcohol consumption are the strongest risk-factors for head and neck carcinogenesis around the world and is the major public health problem in Asian countries. Worldwide, more than 1.1 billion people smoke tobacco. But the incidence of tobacco smoking is high and is ever-increasing in low or middle-income countries like India 8. Despite the fact that use of tobacco and alcohol annually kills more than seven million people, these products are legally sold by manufacturers in all over the world. As per the recent Global Adult Tobacco Survey India Report (2016-2017), more than 199 million smokeless tobacco users are living in India 9. These lifestyle factors play a significant role in the aetiology of HNCs 10. Globally, ~90% of HNCs are associated with avoidable well-known lifestyle factors such as tobacco chewing/smoking and alcohol drinking 11, 12, 13, 14, 15, 16, 17, 18, 19. Regardless of the fact that majority of research studies on HNCs and other diseases are primarily focused on the use of alcohol and tobacco as well-established classical factors, their rates of consumption in many countries specially in low and middle income countries remain high, requiring a better understanding of the mechanisms in HNCs that are exposed to these risk-factors 20. In addition to the carcinogenic effects of tobacco, alcohol, and their metabolites, studies have demonstrated that tobacco products along-with other life style factors (virus/bacterial infections and poor oral hygiene) can directly damage DNA, inducing DNA repair activity. Defective DNA repair can influence and modulate different genetic and epigenetic signalling pathways which effect transcriptional activation, DNA methylation, histone modifications, as well as the altered expression of noncoding RNAs (miRNAs, PIWI-RNAs and LncRNAs etc.), which play critical roles in the genesis of different cancers including HNCs 14, 15, 16, 18.
Noncoding RNAs
Majority of the human genome is transcribed (ENCODE Consortium) and the 20,000 protein-coding genes represent only ⁓2% of the total genome, whereas about 98% is transcribed into RNA that does not code for protein. These non-protein coding RNA molecules comprise of functional RNA molecules 21, 22 which are categorized into housekeeping RNAs and regulatory RNAs 23. The housekeeping RNAs are constitutively transcribed and includes ribosomal (rRNA), transfer (tRNA), small nuclear (snRNA), and small nucleolar RNAs (snoRNAs). The regulatory group of ncRNAs on the other hand are divided into two groups, one that are shorter than 200 nucleotides in length (small ncRNAs) and the ones that greater than 200 nucleotides (long ncRNAs). ncRNA molecules are represented by microRNAs (miRNAs), small interfering RNAs (siRNAs), and PIWI-interacting RNAs (piRNAs), circular RNAs (circRNAs), tRNA-derived small RNAs (tsRNAs) and long ncRNAs (lncRNAs) (Figure 1).
Overview of LncRNAs
Long non-coding RNAs are a highly diverse group of regulatory ncRNAs with respect to characteristics, localization and modes of action 24. LncRNAs are ubiquitously transcribed in the human genome and are emerging as essential players regulating genomic imprinting, shaping chromosome conformation and allosterically regulating enzymatic activity. On the basis of their functions and regulation, lncRNAs are categorised into 3 types, (i) non-functional lncRNAs that are likely to be the result of transcriptional noise, (ii) lncRNAs for which the act of transcription alone is sufficient for their function but the transcript itself is not necessary and (iii) functional lncRNAs that can act in cis and/or in trans25. lncRNAs with a length of >200 nts, are localized in the nucleus. In the nucleus, they modulate transcription by sequestering transcription factors (TFs) or chromatin-modifying enzyme complexes and thus, regulating biological function. The altered expression of lncRNAs is documented as a new hallmark feature in variety of cancers including HNCs 26. Furthermore, disrupted expression of lncRNAs in HNC cells is associated with different stages of cancer and cancer progression (Figure 2).
Figure 2.Dysregulated expression of LncRNAs in head and neck cancer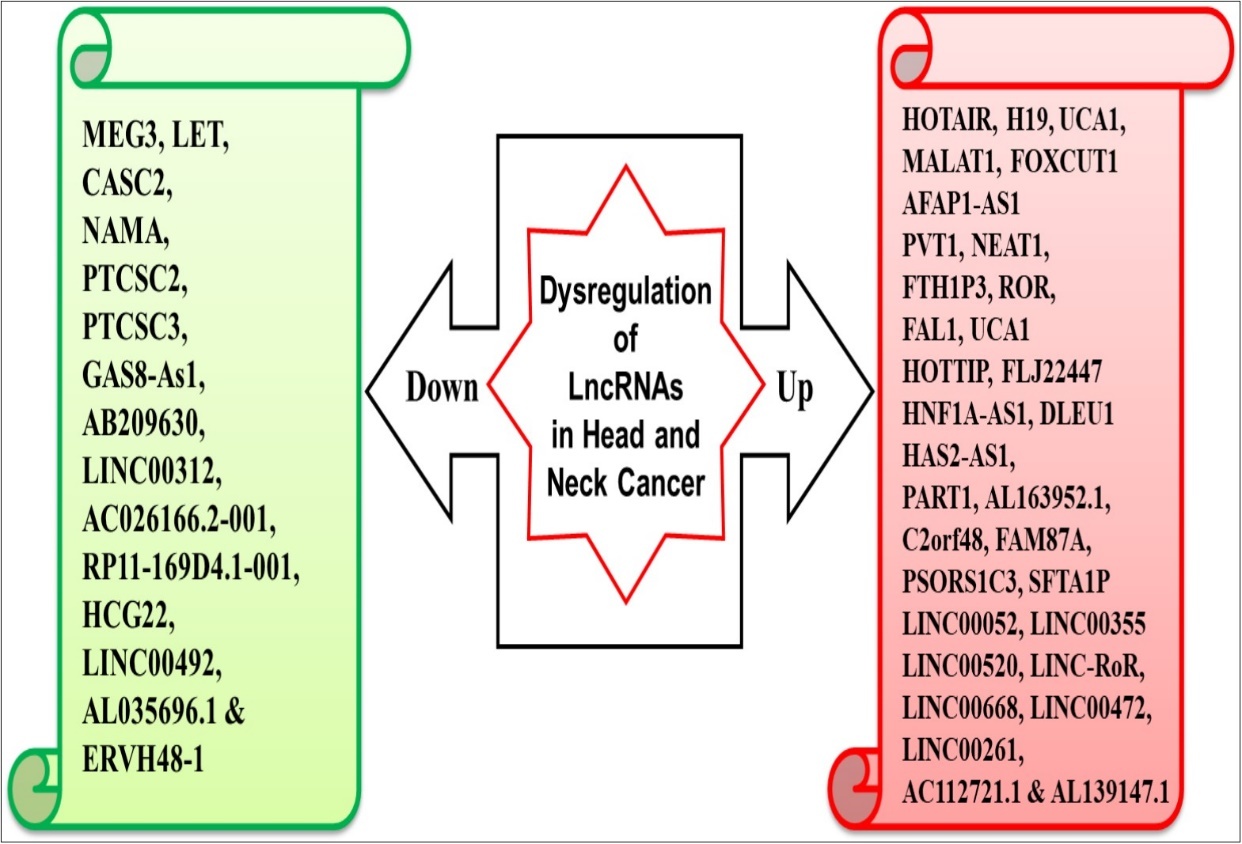
Emerging Role of LncRNAs in Tobacco and/or Alcohol-Induced HNCs
LncRNAs, may act as oncogenic and tumor-suppressive thereby modulating clinical outcome of HNC patients. There are few reports that have found a link between tobacco smoking/alcohol consumption and altered expression of lncRNAs. These lncRNAs regulate molecular processes such cellular differentiation, apoptosis, angiogenesis, proliferation and inflammatory pathways which in turn lead to carcinogenesis 27. The studies on the association between lncRNAs and addiction habits in head and neck cancer are still preliminary and sparse 28, 29.
In a study, Yu and co-workers (2016) demonstrated altered role of lncRNAs in alcohol induced HNC. The authors found the altered expression of lnc-PSD4-1 and lnc-NETO1-1 in alcohol and acetaldehyde induced HNCs 30. In a recent study, expression profiling analysis of lncRNAs showed that 9 out of 11 analysed, were significantly dysregulated in tobacco chewer/smoker HNC patients. Further, altered regulation of linc-RoR ceRNA was observed in undifferentiated tumors which altered treatment response 31. The altered expression level of HOTAIR (HOX transcript antisense RNA) is associated with many types of cancers including oncogenesis, metastasis and poor prognosis in HNC. HOTAIR is emerged as a potential biomarker for HNC diagnosis and prognosis 7, 32, 33, 34. It is reported that polymorphisms could affect the expression of HOTAIR. The rs874945 polymorphism is located in the intron of HOTAIR gene. Recently, rs4759314 polymorphism present in the first intron of HOTAIR, contributes to an increased risk of HNC and serves as a potential biomarker 35. Loss of expression of LINC01133was found in oesophageal cancer tissues and cell lines indicating that it may have an anti-tumor effect in the early grades of oesophageal cancers. Interestingly, LINC01133 expression is markedly lower in patients who were regular drinker and serves as a possible poor prognostic marker and drug target for oesophageal cancers patients 36. Further, alcohol intake has been associated with reduced expression of AC012456.4 in oral cancer patients 37. rs11160608 polymorphism in MEG3 was significantly associated with alcohol-induced oral cancer patients and thus, might play an essential role in oral cancer pathogenesis 38.
LncRNA as Potential Therapeutic Targets
LncRNA expression is altered in various types of cancer. A number of lncRNAs play major roles in HNC metastasis based on their subcellular localization 39. Most of these lncRNAs are located in nucleus and function in chromatin modifications and transcriptional regulation, examples include HOTAIR, MALAT1. On the other hand, lncRNAs such as FOXCUT, CCAT1, LIN00312 and NKILA (Nuclear Factor-kB interacting lncRNA) are localized in the cytoplasm and function as regulator/modulators of mRNA stability, translational controls and protein stability 39.
The above mentioned studies provide evidence for lncRNA as potential therapeutic targets. A number of techniques are available, that target lncRNAs. These have been reviewed by Arun et al., 2018 and include RNAi, antisense oligonucleotides (ASO), CRISPR/Cas, RNA blocking oligonucleotides and small-molecule modulators. RNAi as a therapeutic technique is challenged due to the complexity of in-vivo experiments as well as lack of proper delivery methods. Advancements in ASO chemistry has led to the development of Locked Nucleic Acids (LNA) and S-constrained ethyl (cEt) modifications, which have considerably improved potency and pharmacokinetics profiles 40. Subcutaneously delivered ASO targeting Malat1 in luminal B breast cancer mouse model led to reduction (80%) in metastasis 41. MALAT1 ASO is now being used in many types of metastatic cancers as a potential therapy 42. The engineered CRISPR/Cas13 technique can be used to knockdown the lncRNAs 43. This technique is engineered for mammalian RNA binding and knockdown 43. Small molecules inhibitors may be utilized to target secondary or tertiary structures for lncRNAs, although this technique is still in its infancy 44.
Concluding Remarks
Globally, tobacco smoking/chewing, alcoholism and infection with oncogenic HPV infection are the substantial causative-factors for HNCs. The incidence of tobacco-induced HNCs is increasing in Asian countries such as India, Srilanka, Pakistan and Bangladesh. Due to the intra-oral heterogeneities, differential risk-factors association and diverse etiology of HNCs, it is of great importance to identify novel molecular biomarkers for different subtypes of HNCs which may help to improve the disease outcome and patient survival. Recent discovery of new classes of long non-coding RNAs adds to an amazing complexity of RNA-mediated regulation involved in nearly all biological processes. It is imperative to crack the oncogenic/tumor supressive function of lncRNAs in HNCs with its association with different risk-factors. Thus, proving them to be of great importance in diagnosis, prognosis and treatment of HNC. A curated collection of deregulated lncRNAs in different subtypes of HNC is essential to systematically understand the mechanisms and role of lncRNAs. The mechanism of interaction between lncRNAs and association of specific risk-factors is poorly understood and is still in the initial stage, this poses an obstacle to diagnosis and treatment of different subtypes of HNC. Continuous intensive research with better understanding about specific lncRNA signatures in HNCs associated with differential risk-factors holds great promise to be applied as a prognosticator of HNC and a novel therapeutic target to inhibit HNC metastasis, which will significantly improve HNC patient’s survival rate.
Financial Support & Sponsorship
None.
Acknowledgments
We sincerely thank all authors for their valuable inputs and carefully reading the article.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel R L, Torre L A et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. , CA Cancer J Clin 68, 394-424.
- 2.Johnson N W. (2001) Aetiology and risk factors for oral cancer, with special reference to tobacco and alcohol use. , Magy Onkol 45, 115-22.
- 3.Warnakulasuriya S, Cain N. (2011) Screening for oral cancer: contributing to the debate. , J Investig Clin Dent 2, 2-9.
- 4.Bourhis J, Guigay J, Temam S, Pignon J P. (2006) Chemo-radiotherapy in head and neck cancer. , Ann Oncol. 17 Suppl 10, 39-41.
- 5.Argiris A, Karamouzis M V, Raben D, Ferris R L. (2008) Head and neck cancer. , Lancet 371, 1695-709.
- 6.Dykes I M, Emanueli C. (2017) Transcriptional and Post-transcriptional Gene Regulation by Long Non-coding RNA. , Genomics Proteomics Bioinformatics 15, 177-86.
- 7.Li D, Feng J, Wu T, Wang Y, Sun Y et al. (2012) Long intergenic noncoding RNA HOTAIR is overexpressed and regulates PTEN methylation in laryngeal squamous cell carcinoma. , Am J Pathol 182, 64-70.
- 9.Saha I, Paul B. (2018) War against tobacco: Where do we stand? Indian journal of public health. 62, 55.
- 10.IWGotEoCRt Humans. (2004) World Health O, International Agency for Research on C. Tobacco smoke and involuntary smoking: Iarc;.
- 11.Cogliano V J, Baan R, Straif K. (2011) Updating IARC's carcinogenicity assessment of benzene. , Am J Ind Med 54, 165-7.
- 12.Cogliano V J, Baan R, Straif K, Grosse Y, Lauby-Secretan B et al. (2011) Preventable exposures associated with human cancers. , J Natl Cancer Inst 103, 1827-39.
- 13.Elrefaey S, Massaro M A, Chiocca S, Chiesa F, Ansarin M. (2015) HPV in oropharyngeal cancer: the basics to know in clinical practice. , Acta Otorhinolaryngol Ital 34, 299-309.
- 14.Gupta S, Kumar P, Das B C. (2018) HPV: Molecular pathways and targets. , Curr Probl Cancer 42, 161-74.
- 15.Gupta S, Kumar P, Kaur H, Sharma N, Saluja D et al. (2018) Constitutive activation and overexpression of NF-kappaB/c-Rel in conjunction with p50 contribute to aggressive tongue tumorigenesis. , Oncotarget 9, 33011-29.
- 16.Gupta S, Kumar P, Kaur H, Sharma N, Saluja D et al. (2015) Selective participation of c-Jun with Fra-2/c-Fos promotes aggressive tumor phenotypes and poor prognosis in tongue cancer. , Sci Rep 5, 16811.
- 17.Gupta S, Kumar P, Maini J, Das B C, Bhardwaj M. (2019) PIWI-Interacting RNAs in Oral Cancer: Paradigm Shift in Prognosis and Diagnosis. , J Cancer Sci Ther 11, 086-90.
- 18.Gupta S, Kumar P, Maini J, Kaur H, Das B C. (2018) Epigenetic Biomarkers in Head and Neck Cancer. , Journal of Cancer Genetics and Biomarkers 1, 41.
- 19.Hashibe M, Brennan P, Chuang S C, Boccia S, Castellsague X et al. (2009) Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol Biomarkers Prev. 18, 541-50.
- 20.Beynon R A, Lang S, Schimansky S, Penfold C M, Waylen A et al. (2018) Tobacco smoking and alcohol drinking at diagnosis of head and neck cancer and all-cause mortality: Results from head and neck 5000, a prospective observational cohort of people with head and neck cancer. , Int J Cancer 143, 1114-27.
- 21.Osielska M A, Jagodzinski P P. (2018) Long non-coding RNA as potential biomarkers in non-small-cell lung cancer: What do we know so far? Biomed Pharmacother. 101, 322-33.
- 22.Ponting C P, Belgard T G. (2010) Transcribed dark matter: meaning or myth?. , Hum Mol Genet 19, 162-8.
- 23.Palazzo A F, Lee E S. (2015) Non-coding RNA: what is functional and what is junk?. , Front Genet 6, 2.
- 24.Kung J T, Colognori D, Lee J T. (2013) Long noncoding RNAs: past, present, and future. , Genetics 193, 651-69.
- 25.Quinn J J, Chang H Y. (2015) Unique features of long non-coding RNA biogenesis and function. , Nat Rev Genet 17, 47-62.
- 26.Prensner J R, Chinnaiyan A M. (2011) The emergence of lncRNAs in cancer biology. , Cancer Discov 1, 391-407.
- 27.N Soares do Amaral, EMN Cruz, B de Melo Maia, Malagoli Rocha R. (2016) Noncoding RNA Profiles in Tobacco- and Alcohol-Associated Diseases. Genes (Basel).8.
- 28.Pentenero M, Bowers L, Jayasinghe R, Cheong S C, Farah C S et al. (2019) World Workshop on Oral Medicine VII: Functional pathways involving differentially expressed lncRNAs in oral squamous cell carcinoma. , Oral Dis.25 Suppl 1, 79-87.
- 29.Pentenero M, Bowers L M, Jayasinghe R, Yap T, Cheong S C et al. (2019) World Workshop on Oral Medicine VII: Clinical evidence of differential expression of lncRNAs in oral squamous cell carcinoma: A scoping review. Oral Dis. 25, 88-101.
- 30.Yu V, Singh P, Rahimy E, Zheng H, Kuo S Z et al. (2016) RNA-seq analysis identifies key long non-coding RNAs connected to the pathogenesis of alcohol-associated head and neck squamous cell carcinoma. , Oncol Lett 12, 2846-53.
- 31.Arunkumar G, AK Deva Magendhra Rao, Manikandan M, Arun K, Vinothkumar V et al. (2017) Expression profiling of long non-coding RNA identifies linc-RoR as a prognostic biomarker in oral cancer. , Tumour Biol 39, 1010428317698366.
- 32.Lee M, Kim H J, Kim S W, Park S A, Chun K H et al. (2016) The long non-coding RNA HOTAIR increases tumour growth and invasion in cervical cancer by targeting the Notch pathway. , Oncotarget 7, 44558-71.
- 33.Nie Y, Liu X, Qu S, Song E, Zou H et al. (2013) Long non-coding RNA HOTAIR is an independent prognostic marker for nasopharyngeal carcinoma progression and survival. , Cancer Sci 104, 458-64.
- 34.Zhou X, Chen J, Tang W. (2014) The molecular mechanism of HOTAIR in tumorigenesis, metastasis, and drug resistance. , Acta Biochim Biophys Sin (Shanghai) 46, 1011-5.
- 35.Wu B, Liu J, Wang B, Liao X, Cui Z et al. (2018) Association on polymorphisms. in LncRNA HOTAIR and susceptibility to HNSCC in Chinese population. Eur Rev Med Pharmacol Sci 22, 702-6.
- 36.Yang X Z, He Q J, Cheng T T, Chi J, Lei Z Y et al. (2018) . Predictive Value of LINC01133 for Unfavorable Prognosis was Impacted by Alcohol in Esophageal Squamous Cell Carcinoma. Cell Physiol Biochem 48, 251-62.
- 37.Hu X, Qiu Z, Zeng J, Xiao T, Ke Z et al. (2018) A novel long non-coding RNA, AC012456.4, as a valuable and independent prognostic biomarker of survival in oral squamous cell carcinoma. , PeerJ 6, 5307.
- 38.Hou Y, Zhang B, Miao L, Ji Y, Yu Y et al. (2019) Association of long non-coding RNA MEG3 polymorphisms with oral squamous cell carcinoma risk. Oral Dis. 25, 1318-24.
- 39.Luo X, Qiu Y, Jiang Y, Chen F, Jiang L et al. (2018) Long non-coding RNA implicated in the invasion and metastasis of head and neck cancer: possible function and mechanisms. , Mol Cancer 17, 14.
- 40.Arunkumar G, Anand S, Raksha P, Dhamodharan S, H Prasanna Srinivasa Rao et al. (2018) LncRNA OIP5-AS1 is overexpressed in undifferentiated oral tumors and integrated analysis identifies as a downstream effector of stemness-associated transcription factors. , Sci Rep 8, 7018.
- 41.Arun G, Diermeier S, Akerman M, Chang K C, Wilkinson J E et al. (2015) . Differentiation of mammary tumors and reduction in metastasis upon Malat1 lncRNA loss. Genes Dev 30, 34-51.

