Virtual Reality in the Care of People with Dementia: A Single-Case Research Study
Abstract
More than 90% of people with dementia develop behavioral and psychological symptoms of dementia. First-line care strategies in dementia care should consider a combination of pharmacological and non-pharmacological interventions. The present single-case research study aimed to evaluate the use of virtual reality in the context of behavioral and psychological symptoms of dementia, quality of life, and medication use among people with dementia. Ten persons with dementia used virtual reality for a mean of twice per week for eight weeks. In each virtual reality session, lasting for a maximum of 30 minutes, the persons with dementia chose one to three short films from 11 different films: a hen run, a farm with animals, two cafés, an old-fashioned grocery shop, a local river, a square in the local city, a museum, a castle, a fishing boat and an Austrian mountain scenery. Quantitative and qualitative data were collected pre-, during, and post-intervention. No major differences in the quantitative data in terms of behavioral and psychological symptoms of dementia, quality of life, or medication use were observed. However, the qualitative data showed that the use of virtual reality provided the persons with dementia with short-term enjoyment, heightened energy and alertness, and an experience of reminiscence. The use of virtual reality may therefore serve as a complementary tool to the existing non-pharmacological management techniques of people with dementia in nursing homes.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC , Macedonia.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Annelie K. Gusdal, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Dementia is an increasingly prevalent chronic condition that affects an estimated 50 million people worldwide. With nearly 10 million new cases every year, dementia raises significant challenges within healthcare and social-care systems 1. People with dementia (PwD) experience a progressive loss of cognition and will gradually develop responsive behaviors, also referred to as behavioral and psychological symptoms of dementia (BPSD). More than 90% of PwD will ultimately develop BPSD during the trajectory of the disease 2. BPSD has been defined as the “signs and symptoms of disturbed behavior, mood, thought, or perception” 3. There is a risk that BPSD may result in physical injuries and psychological distress in PwD and their caregivers, and such symptoms have been identified as predictors of nursing home placement 4. In nursing homes, verbal and physical abuse from PwD exhibiting BPSD has been reported by care staff, which may result in minimized contact with the PwD and a reduction in their quality of care 3.
Antipsychotic medication is commonly prescribed for PwD’s BPSD, although it has been reported to exhibit low efficacy while also being associated with adverse effects 5, 6, bringing into focus the potential for environmental, behavioral, and lifestyle interventions to enhance the well-being and cognitive function of PwD. Hence, first-line strategies in care should not expeditiously be pharmacological interventions; rather, consideration should be given to a combination of pharmacological and non-pharmacological interventions to avert or reduce BPSD while considering the PwD’s unique needs 7, 8.
Recent systematic reviews have identified and reported the positive effects of non-pharmacological interventions on BPSD and quality of life 7, 8, 9, 10, 11, 12, 13, 14 with the intention to promote quality care, dignity, and safety for PwD. These non-pharmacological interventions have been shown to have positive effects on anxiety, depression, and agitated behavior, and such approaches include physical activity; different forms of sensory-focused interventions such as music-, aroma-, massage- and light-based therapies; skills training and education in person-centered care for the care staff; and environmental redesigning 7, 10.
Virtual reality (VR) is an additional, and relatively novel, non-pharmacological intervention in dementia care. VR is a technology that digitally delivers a three-dimensional environment, allowing people to interact within it and provide sensory inputs. VR can be presented at different levels of immersion, which facilitates a sense of presence in the virtual world 15. A majority of the systematic reviews, intervention case studies, and single-case research studies on the use of VR have reported promising results with respect to promoting PwD’s cognitive functions, in terms of episodic memory, dual tasking, spatial navigation, and visual attention 16, 17, 18, 19, 20, 21, 22, 23, 24, 25. VR has also been used successfully as exposure therapy in the management of PwD’s pain and stress 26. Furthermore, improvements in PwD’s psychological functioning, in terms of reduction of anxiety, increased well-being and quality of life, have also been reported 27, 28, 29, 30. However, in this latter strand of research on PwD’s psychological functioning, none of the studies have implemented validated quality of life questionnaires or several VR sessions over a longer period. More specifically, Ferguson et al. 27 and Moyle et al. 28 limited the experience of VR to a single session. As a response to the scarcity of reiterative and lengthy evaluations of VR in the care of PwD, the present study aimed to evaluate the use of VR in terms of its effects on BPSD, quality of life, and medication use during an eight-week intervention period among PwD. The secondary aim was to describe the care staff’s experiences with respect to the usability and feasibility of VRin their care of PwD in a nursing home setting.
Materials and Methods
Design
A single-case research (SCR) study with an A-B-A design was conducted, in which the participants served as their own controls 31, 32, 33, 34. Phase A1 was comprised of a baseline/pre-intervention period of three weeks. Phase B consisted of an eight-week intervention with the use of VR (Samsung Gear VR - SM-R323 - headset) 35, and phase A2 involved the post-intervention, conducted during two weeks after the completion of the intervention in phase B.
Setting and Participants
The present study was conducted in an eight-unit nursing home in Sweden during the period of September through to December of 2019. In total, six female PwD, four male PwD, and 19 care staff from four different dementia care units participated in the study. The demographic information of the PwD and care staff is summarized in Table 1 and Table 2, respectively. The inclusion criteria for the PwD were a diagnosis of dementia and having BPSD, while those for the care staff were to be a contact person for the eligible PwD or possessing considerably strong knowledge of them.
Table 1. Demographic data of the PWD| PwD (n = 10) | Sex | Age (years) | Dementia diagnosis and progression |
| PwD 1 | M | 73 | AD, moderate |
| PwD 2 | M | 81 | Unspecified, moderate |
| PwD 3 | F | 78 | AD, moderate |
| PwD 4 | M | 62 | Unspecified, moderate |
| PwD 5 | F | 77 | VaD, moderate |
| PwD 6 | F | 79 | VaD, moderate |
| PwD 7 | F | 88 | Unspecified, moderate |
| PwD 8 | F | 85 | VaD, moderate |
| PwD 9 | M | 77 | Unspecified, moderate |
| PwD 10 | F | 73 | Unspecified, moderate |
| Care staff (n = 19) | |
| Sex (female/male) | 19/0 |
| Median age in years (range) | 50 (32–63) |
| Median years of experience at the current nursing home (range) | 9 (3–9) |
Recruitment
The care staff informed 11 eligible PwD in their respective care units as well as their respective next of kin or trustees, both verbally and in writing, of the background and purpose of the study. They were also informed that the participation of the PwD was voluntary, and that they could withdraw their participation if, and whenever, they wished to. In total, 11 PwD commenced the study after their next of kin or trustee signed a statement that they did not oppose the PwD’s participation in the study. Since obtaining signed informed consent was not possible from nine of the PwD, the assent/dissent process was carefully considered throughout the study; participation assent was obtained from the PwD at the beginning of each VR session. One PwD withdrew halfway into the study due to unknown reasons underlying a repeated refusal to experience VR. At the completion of the intervention, 19 care staff members were asked to participate in group interviews; ten care staff members participated after receiving verbal and written information regarding the interviews and signing the informed consent forms.
Intervention
Content
The VR apparatus (Figure 1) in the present study consisted of the following equipment: (1) Hardware included a network connection for data traffic, a computer, and VR glasses (in this case the Samsung Gear VR - SM-R323 - headset); (2) Software included VR films supplied by the company from which the equipment was leased (Atea Sverige AB).
Delivery
The intervention was performed for a total duration of eight weeks (study weeks: 4–11), during which ten PwD used the VR for a mean of twice per week (Table 3). The VR sessions began with the care staff leading the PwD to the assigned room, approximately 100–200 meters from the four care units. The assigned room was furnished with a comfortable armchair for the PwD, a regular chair for the care staff, and the VR equipment. Each VR session was limited to a 30-minute duration based on recommendations in published VR methodology 36. The overall time scheduled was one hour, which allowed for 15 minutes to walk from the care unit to the VR room, the VR session for 30 minutes, and then the walk back to the care unit. In each VR session the PwD chose one to three short films from 11 different films: a hen run, a farm with animals, two cafés, an old-fashioned grocery shop, a local river, a square in the local city, a museum, a castle, a fishing boat and Austrian mountain scenery. The care staff member asked which of the 11 films the PwD preferred to watch. If the PwD did not have a preference, the care staff member started a randomly selected film, and if the PwD seemed to enjoy it, the film was continued. If not, the care staff member switched to another film. The films did not involve crowds, sudden noises, or sudden scene changes. The PwD could rotate his or her head 360 degrees and still remain immersed in the scene.
Table 3. Total number of undertaken vs. denied VR sessions| Person with dementia (PwD) | Total number of undertaken VR sessions | Total number of denied VR sessions |
| PwD 1 | 16 | 0 |
| PwD 2 | 16 | 0 |
| PwD 3 | 16 | 0 |
| PwD 4 | 13 | 3 |
| PwD 5 | 15 | 1 |
| PwD 6 | 14 | 2 |
| PwD 7 | 11 | 5 |
| PwD 8 | 16 | 0 |
| PwD 9 | 12 | 4 |
| PwD 10 | 13 | 3 |
Data Collection
The present SCR study consisted of the collection of quantitative and qualitative data pre-intervention (Phase A1), during the intervention (Phase B), and post-intervention (Phase A2). Table 4 presents an overview of the data collection. The first author provided support to and training of the care staff regarding the data collection, both prior to the study and during the study on a weekly basis.
Table 4. Overview of the data collection pre-intervention, during the intervention, and post-intervention| Pre-intervention | Intervention | Post-intervention | |||||||||||||||||
| Study weeks | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||||||
| Demographic data | x | x | |||||||||||||||||
| BPSD (NPI-NH) | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||
| QUALID | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||
| Medication use | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||
| Care staff’s notes | x | x | x | x | x | x | x | x | |||||||||||
| Group interviews with care staff | x | ||||||||||||||||||
Quantitative data - Assessment Instruments and Medication Use
The Neuropsychiatric Inventory – Nursing Home Version (NPI-NH) scale 37, 38 was used by the care staff for assessing the PwD’s BPSD (dependent variables) pre-intervention, during the intervention, and post-intervention. The NPI-NH is comprised of 12 items, including the following neuropsychiatric symptoms: delusions, hallucinations, agitation, depression, anxiety, euphoria, apathy, disinhibition, irritability, aberrant motor behavior (restlessness and wandering), night-time behavior (sleep) disturbances, and appetite and eating disorders; for each of these 12 items, the presence, frequency, and severity is assessed, and the score for each neuropsychiatric symptom is obtained by multiplying the severity (range: 1–3) by the frequency (range: 1–4). The summed symptom scores provide the total NPI-NH score, which ranges from 0 to 144. The NPI-NH data were collected three times/week during the three-week pre-intervention to achieve a steady base line, once biweekly during the eight-week intervention, and once during the two-week post-intervention.
The Quality of Life in Late-Stage Dementia (QUALID) scale 39, 40 was used by the care staff for assessing the PwD’s quality of life (dependent variables) pre-intervention, during the intervention, and post-intervention. The QUALID is comprised of 11 items, including the following behaviors: smiling, sadness, crying, emotional discomfort, physical discomfort, discontent, irritability/aggression, appetite, enjoying physical contact, enjoying social contact, and appearing calm and relaxed. The 11 statements are ranked on a five-point scale. The summed scores range from 11 to 55, with lower scores representing a higher quality of life. QUALID data were collected three times/week during the three-week pre-intervention to achieve a steady base line, once biweekly during the eight-week intervention, and once during the two-week post-intervention.
Data on the PwD’s medication use regarding benzodiazepine derivatives and benzodiazepine-related agents were noted in the research protocol by the registered nurse in charge of the respective care unit. The data on medication use was collected by the researchers weekly pre-intervention, during the intervention, and post-intervention.
Qualitative data - Care Staff’s Notes and Group Interviews
Care staff’s notes, which were written in conjunction with each VR session and included observations of the PwD’s reactions and opinions (both verbal and non-verbal), were collected during the eight-week intervention. Group interviews were conducted post-intervention to explore the overall experiences of the care staff regarding the use of VR in their care for PwD. A semi-structured interview guide (Table 5) was used, which consisted of an initial open-ended question, followed by targeted questions 41. Follow-up and probing questions were included for clarification when required. Four group interviews were conducted with ten care staff members within their respective care units, with each interview lasting for 17–20 minutes. All the interviews were conducted by the first author, recorded digitally and transcribed verbatim.
Table 5. Interview guide for group interviews with care staff| What was your overall experience of using VR in the care of PwD? |
| Has the use of VR contributed to a change in the PwD’s BPSD, and if so, how? |
| Has the use of VR contributed to a change in the PwD’s quality of life, and if so, how? |
| In what situations (how, when, and why) did you choose to use VR: at a certain time of day, during specific BPSD in the PwD, or for some other reason? |
| Did you encounter specific difficulties in using VR, and if so, what were they? |
| How did you perceive the feasibility of using VR? |
| What are your thoughts about the eventual future use of VR? |
Data Analyses
Quantitative data - Assessment Instruments and Medication Use
Quantitative data from the NPI-NH and QUALID scales were analyzed through visual inspection and descriptive statistics. Visual inspection consisted of the calculation of each participant’s performance, which was graphed to visually determine the data’s (1) trend or progress over time, (2) the level or magnitude, and (3) the variability vs. stability 32. The visual inspection procedure followed the six steps outlined by Lane and Gast 42 using the graphic display and the split-middle method of dividing the data into within-condition and between-condition data analyses. Stability was defined as 80% of the data points being within ± 25% of the phase median.
Qualitative Data - Care Staff’s Notes and Group Interviews
Qualitative data from care staff’s notes and group interviews were summarized using qualitative content analysis with a descriptive approach 41. The qualitative description was used to present the variations in the experiences of care staff regarding the use of VR in the care of PwD.
Ethical Considerations
The present study was approved by the Regional Ethical Review Board in Uppsala (Dno. 2019/00252) and conformed to the principles outlined in the Declaration of Helsinki 43 and in the Recommendations for the Protection of Research Participants by the International Committee of Medical Journal Editors 44.
Results
The detailed results and the respective graphs for each of the ten PwD’s BPSD, quality of life, and medication use together with care staff’s notes are presented. Further, the findings from the group interviews regarding the care staff’s experiences of the usability and feasibility of VR in the care of PwD are described. An overview of both quantitative and qualitative results is presented in Table 6.
Table 6. Overview of PwD’s BPSD, quality of life, medication use, enjoyment, energy and alertness, reminiscence, topics of conversation at post-intervention.| PwD | Improvement of BPSD | Worsening of, or no change in, BPSD | Increased quality of life | Decreased, or no change in, quality of life | Change in medication use | Heightened enjoyment | Increased energy and alertness | Reminiscence | New topics of conversation |
| 1 | x | x | x | x | x | x | |||
| 2 | x | x | x | x | x | x | |||
| 3 | x | x | x | x | x | ||||
| 4 | x | x | x | x | |||||
| 5 | x | x | |||||||
| 6 | x | x | x | x | x | x | |||
| 7 | x | x | x | x | x | ||||
| 8 | x | x | x | x | x | x | |||
| 9 | x | x | x | x | x | ||||
| 10 | x | x | x | x | x | x | x |
PwD’s BPSD, Quality of Life, Medication Use, and Care Staff’s Notes
PwD 1
For PwD 1, there was an assessed presence and change in BPSD in terms of irritability, along with an assessed change in the quality of life (Figure 2). The split-middle method for trend estimation indicated an overall zero-celerating trend for BPSD and a decelerating trend for quality of life during the pre-intervention. During the intervention, a zero-celerating trend for BPSD and quality of life was observed. Mean, median, and relative change measures indicated an improvement of BPSD and an increased quality of life from pre-intervention to intervention. Data for BPSD and quality of life were stable. There was no medication use during the study.
Figure 2.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 1. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show the measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.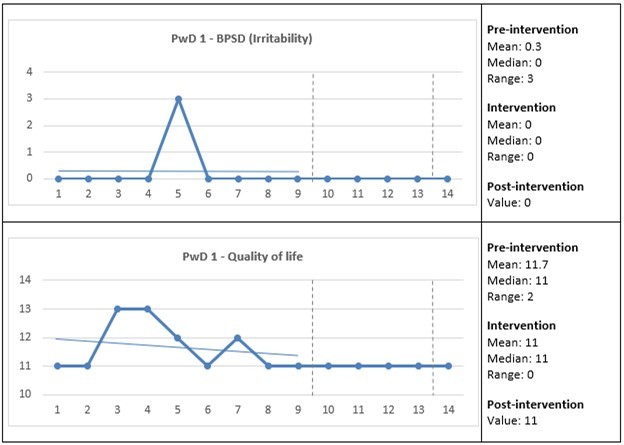
Care staff described in notes that the person was very amused, active, and alert while experiencing VR. He was also reported to be attentive to details, given that “… he heard sounds that came from far, for example, a train, a man who walked on gravel, a cyclist who swished past, and sounds from different types of weather.” This person also recognized several places and recounted memories from his childhood. For instance, it was reported, “He thought it was a shame that the city square was changed and that the round kiosk was torn down. ‘My mother and I have eaten a lot of good stuff there,’ he said.” PwD 1 was interested in all the different VR films and was especially fascinated by the hen run and other films with animals, together with films from the local area that he was familiar with. He gladly described his experiences afterwards to other care staff and looked forward to the next VR session.
PwD 2
For PwD 2, there was an assessed presence of and change in BPSD in terms of irritability, along with an assessed change in the quality of life (Figure 3). The split-middle method for trend estimation indicated an accelerating trend for BPSD and quality of life during the pre-intervention. During the intervention, a zero-celerating trend for BPSD and an accelerating trend for quality of life were observed. Mean, median, and relative change measures indicated an improvement of BPSD and an increased quality of life from pre-intervention to intervention. Data for BPSD and quality of life were stable. There was no change in medication use during the study.
Figure 3.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 2. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show the measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.
Care staff described in notes that the person experienced slight dizziness during the first VR session, and the care staff stopped the film and helped him to take off the VR glasses. This dizziness was not experienced again in the coming sessions. He was interested in all the films and became very enthusiastic about the footage and filmmaking of the scenery in Austria. He recounted memories from the times he had visited the country and showed with his hands how he had filmed the scenery himself while in Austria. He was also attentive to details, as it was reported that “… he listened to the water rippling through the village and the apple-trees full of apples.”He was keen to show the films to his children the next time they came to visit. He asked several questions about the background of the films and wanted to prolong the VR sessions each time. He was always looking forward to the next VR session.
PwD 3
For PwD 3, there was an assessed presence of and change in BPSD in terms of irritability and appetite and eating disorders, along with an assessed change in the quality of life (Figure 4). The split-middle method for trend estimation indicated an accelerating trend for BPSD and quality of life during the pre-intervention. During the intervention, an accelerating trend for BPSD and quality of life was observed. Mean, median, and relative change measures indicated a worsening of BPSD, and an increased quality of life from pre-intervention to post-intervention. Data for BPSD and quality of life were stable. There was no change in medication use during the study.
Figure 4.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 3. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show the measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.
Care staff described in notes that the person was curious and looked forward to each VR session. She only enjoyed the films of the hen run and children swimming, while the other films were considered boring or gray. The hen run brought several memories back to life that the care staff had not previously heard. For instance, “… she described the hens that her neighbor kept when she was a child and described in detail the difference and meaning of the crest on the hen’s and rooster’s head.” She requested films from churches as she wanted to enjoy the interior beauty of them, but since there was a lack of these films, she instead talked at length with the accompanying care staff about the beauty and history of her childhood village, in which she lived until the age of nine, and its magnificent church. A couple of times, she experienced discomfort from the VR glasses and had to take them off for a while, and then put them back on again.
PwD 4
For PwD 4, there was an assessed presence of and change in BPSD in terms of agitation and disinhibition, along with an assessed change in the quality of life (Figure 5). The split-middle method for trend estimation indicated an accelerating trend for BPSD and a decelerating trend for quality of life during the pre-intervention. During the intervention, a zero-celerating trend for BPSD and quality of life was observed. Mean, median, and relative change measures indicated an improvement of BPSD and no change in quality of life from pre-intervention to post-intervention. Data for BPSD and quality of life were stable. There was no medication use during the study.
Figure 5.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 4. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show the measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.
Care staff described in notes that the person at first was amused by all the films, especially the hen run, as he would “… call out to the hens, stretching out his hands toward them.” When he saw a bicycle leaned toward a fence, he told the care staff how much he had always enjoyed cycling. In the café, he “… laughed when he tried to reach for a cookie but didn’t get it.” When watching films from the local area, he was positively surprised to see newly built houses and recounted memories attached to the different places, e.g., “… today we started with the castle, and he told me that his cousin got married there.”However, he gradually lost interest in the VR sessions as the films became boring and too slow. Thus, he decided against going to three VR sessions in the last two intervention weeks.
PwD 5
For PwD 5, there was an assessed presence of and change in BPSD in terms of appetite and eating disorder, along with an assessed change in the quality of life (Figure 6). The split-middle method for trend estimation indicated an accelerating trend for BPSD and quality of life. During the intervention, a zero-celerating trend for BPSD and a decelerating trend for quality of life were observed. Mean, median, and relative change measures indicated a worsening of BPSD and a decreased quality of life from pre-intervention to post-intervention. Data for BPSD and quality of life were stable. There was no change in medication use during the study.
Figure 6.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 5. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.
Care staff described in notes that this individual at most times became quickly bored, even when watching her favorite film about kittens. According to one staff member, “I asked her to tell me what she saw, but she shrugged her shoulders and said, ‘Yeah, nothing special’.” At most times, she did not have any suggestions on which films she wanted to see, and only a few minutes into each film, she lost interest and asked the care staff to either change it or help her to the toilet. She decided against one VR session and turned around in the door on her way into the VR room, remarking, “… this is not fun. I don’t want to. Take me back.” She could not, or more likely did not want to, recall what she had seen after each session, except for the animals and nature in a film about camping in Austria.
PwD 6
For PwD6, there was an assessed presence of and change in BPSD in terms of delusions, agitation, depression, anxiety, disinhibition, irritability, and aberrant motor behavior, along with an assessed change in the quality of life (Figure 7). The split-middle method for trend estimation indicated a decelerating trend for BPSD and quality of life during the pre-intervention. During the intervention, an accelerating trend for BPSD and quality of life was observed. Mean, median, and relative change measures indicated a worsening of BPSD and an increased quality of life from pre-intervention to post-intervention. Data for BPSD and quality of life were stable. There was no change in medication use during the study.
Figure 7.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 6. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.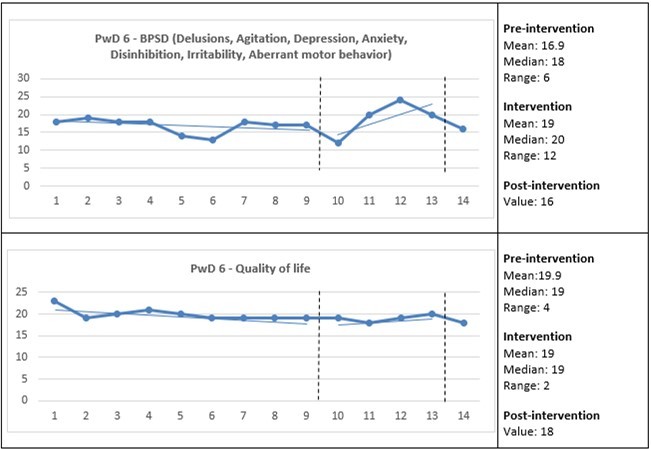
Care staff described in notes that this individual was very amused and active while experiencing VR. For instance, she laughed loudly when watching the man who was jig fishing lay himself down in the snow and when visiting the virtual café. One staff member reported hearing“… loud laughter when she actively tried to get hold of the coffee cup and the cake, and she wondered who was teasing her like this. She looked up to the sky several times; she was fascinated by the big birds and wondered if she was in the Old Town in Stockholm.”She also enjoyed hearing children’s laughter in the film from Austria, but the film with rushing water was frightening for her, as she was afraid to fall in the water. After each VR session, she thanked the staff for the opportunity to watch the films. According to the notes, “She was fascinated with this whole experience with these glasses that let her see so many new things.” She also enjoyed the films from the local areas in which she recognized buildings and scenery. The film of the hen run brought back old memories that she recounted afterwards. Also, the films with cows and kittens inspired her. According to one report, “… she was very happy and enjoyed seeing the animals. She was in a good mood afterwards and recounted several times what she had just seen.” She decided against participating in two VR sessions, once due to being restless (as she had aberrant motor behavior) and once due to worry about her husband.
PwD 7
For PwD 7, there was an assessed presence of and change in BPSD in terms of delusions, agitation, and apathy, along with an assessed change in the quality of life (Figure 8). The split-middle method for trend estimation indicated an accelerating trend for BPSD and quality of life during the pre-intervention. During the intervention, a zero-celerating trend for BPSD and an accelerating trend for quality of life were observed. Mean, median, and relative change measures indicated a worsening of BPSD and a decreased quality of life from pre-intervention to intervention. Data for BPSD and quality of life were stable. There was no change in medication use during the study.
Figure 8.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 7. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.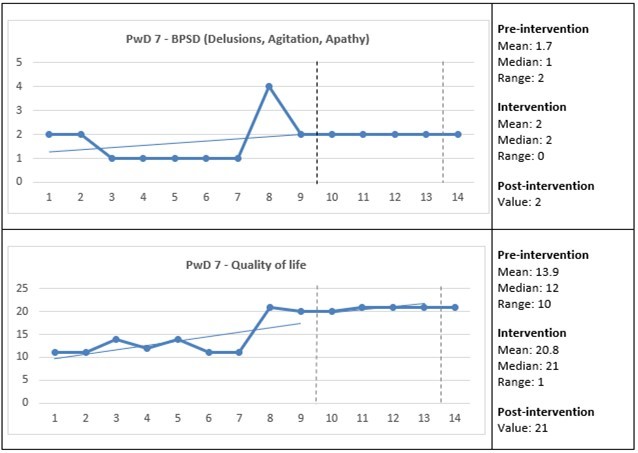
Care staff described in notes that the person enjoyed the beauty and reminisced when watching the river running through her childhood hometown. When watching the man jig fishing, it was reported that“… she laughed loudly when he waived his fishing rod right in front of her.” The hens in the hen run amused her when they were close and seemed to pick on her feet; she also talked happily to the rooster. In the film from Austria, she enjoyed hearing the children and was fascinated by the lush green scenery. In the antique café, she was “… tempted by plenty of nice pastries. When we had watched this for some time, she said, ‘Now I want to go back and have a cup of coffee after seeing so many goodies’.” Most days, this individual preferred to lie in bed all day, but the VR session was the motivator for her to get out of bed and get dressed. She decided against five VR sessions as she was either too tired, had caught a cold, or was in a bad mood. Post-intervention, the care staff noticed that she was more difficult to motivate and seemed less happy.
PwD 8
For PwD 8, there was an assessed presence of and change in BPSD in terms of delusions and anxiety, along with an assessed change in the quality of life (Figure 9). The split-middle method for trend estimation indicated a decelerating trend for BPSD and an accelerating trend for quality of life during the pre-intervention. During the intervention, an accelerating trend for BPSD and a zero-celerating trend for quality of life were observed. Mean, median, and relative change measures indicated a worsening of BPSD, and there was no change in quality of life from pre-intervention to intervention. Data for BPSD and quality of life were stable. There was no change in medication use during the study.
Figure 9.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 8. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.
Care staff described in notes that this individual happily enjoyed the scenic nature films. She vividly spoke about the beautiful views, indicating how fantastic it was to get so close to the scenery, and that she had learned about the plants and trees while watching and talking about them. The films also distracted her from previous sad thoughts. According to one report, “… before watching the film, she was a little sad because of another resident, but now, she said, ‘I can watch and watch and not think of the sad things’.” One of the films had rhythmic and joyful music that brought her to dance (while sitting down) and clap her hands. In one staff member’s notes, it was reported that “… several times she said that this film made her body sparkle and her soul happy. ‘I can’t sit still, I can’t sit still,’ she said as she laughed.” When watching the films with animals on a farm, “… she remembered her childhood when she was with her parents in their summer cottage. She told me that it was wonderful in the countryside with its fresh air, and that she was happy in those days.” When watching films shot in the local area, she recognized and remembered the names of several places, which was surprising for the care staff. After each VR session, she looked forward to the next one.
PwD 9
For PwD 9, there was an assessed presence of and change in BPSD in terms of agitation, irritability, and appetite and eating disorder, along with an assessed change in the quality of life (Figure 10). The split-middle method for trend estimation indicated a decelerating trend for BPSD and an accelerating trend for quality of life during the pre-intervention. During the intervention, a decelerating trend for BPSD and an accelerating trend for quality of life were observed. Mean, median, and relative change measures indicated an improvement of BPSD and an increased quality of life from pre-intervention to intervention. Data for BPSD and quality of life were stable. There was no change in medication use during the study.
Figure 10.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 9. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.
Care staff described in notes that during the first VR sessions, this individual experienced dizziness and felt as though he was high up in the air and falling, irrespective of which film he watched. When experiencing dizziness, he would quickly remove the glasses and continue watching on the screen instead. After the initial VR sessions, his dizziness gradually subsided, and he enjoyed the films of the virtual café, the jig fishing, and the hen run. According to the notes, “he commented on the brand of the car that was parked on the farm and on the bicycle, and he considered it to be crazy to park the bicycle inside the hen run.” When watching the jig fishing, he described his previous experiences of fishing, which he had enjoyed a lot. He was interested in and fascinated by the actual data animation and construction of the VR films with computers, which care staff associated with his former profession as an engine designer and constructer. He decided against participating in four VR sessions for unknown reasons.
PwD 10
For PwD 10, there was an assessed presence of and change in BPSD in terms of irritability, along with an assessed change in the quality of life (Figure 11). The split-middle method for trend estimation indicated a decelerating trend for BPSD and quality of life during the pre-intervention. During the intervention, a decelerating trend for BPSD and an accelerating trend for quality of life were observed. Mean, median, and relative change measures indicated a worsening of BPSD and an increased quality of life from pre-intervention to intervention. Data for BPSD and quality of life were stable. There was a change in medication use as the person had contracted a urinary tract infection during the study.
Figure 11.Care staff assessed the presence and change in the behavioral and psychological symptoms of dementia (BPSD) and quality of life for PwD 10. The Y-axes show the total scores for the BPSD and quality of life, and the X-axes show measurement points: 1–9 = three weeks pre-intervention; 10–13 = four weeks intervention; and 14 = one-week post-intervention (see also vertical dashed lines). Horizontal lines represent trend lines for pre-intervention and intervention. PwD = Person with dementia.
Care staff described in notes that the person was thrilled about the films from the start, and that she understood how to move her head to change her view of the film. It was important to her that she was in the same VR room and did not alternate between the two different VR rooms. When watching the film of the hen run, she directly started to talk about her grandmother in Finland. The memories from Finland were again brought up when watching the scenery of a lake, during which it was reported that“… she told me that as a child in Finland, she lived by a lake where she had a view of three islands in the lake.” Each film brought memories to life for this individual. For example, the scenery from Austria reminded her of her brother’s home in northern Sweden, and the café reminded her of a job she once had, during which “… she interacted joyfully with the waitress, and she laughed and said that she could not buy anything because she had not brought any money.” The film from the mushroom forest reminded her of a mushroom sauce recipe she used to prepare when her children were small. When she interacted with the VR films, she spoke Swedish, which surprised the care staff as she normally talked to herself, and others, in Finnish. On several occasions when starting the VR session, she was restless, indicating that she had to go to the dentist or to the bathroom. A urinary tract infection was soon found to be the reason for her restlessness, which also caused her to miss two VR sessions, but after medical treatment, she became calmer and mostly enjoyed the films again.
Care Staff’s Experiences Regarding the Usability and Feasibility of VR
The care staff’s overall experience with using VR in the care of PwD was very positive, as they felt that they had generally contributed to joyful experiences for the PwD while also catching a new glimpse of the PwD’s personalities and previous lives.
However, the care staff acknowledged that VR had not contributed to any lasting changes in the PwD’s BPSD and quality of life. Rather, the changes were temporary and in close conjunction with the VR session. In one unit, a care staff member expressed the temporary nature of the changes as follows:
No, no changes over time. But right now, they are doing well. // So, it’s probably just for the moment, but it’s been a cozy moment. Then, maybe it has lasted a while. // For one man, it might be an hour, or one and a half afterwards, and for the other man, it lasts throughout the afternoon, evening, and maybe a whole day. // He’s happier and doesn’t react so strongly to negative things in the care unit, I would say.
The temporary beneficial changes were perceived in the PwD’s heightened sense of joy in the moment and their lively associations with their child- and adulthood. It was not entirely clear whether some PwD remembered the films afterwards, but this was not viewed as important if a positive and pleasant feeling was considered to have lingered inside the PwD after the VR sessions.
Prerequisites for conducting the study were meticulous staff planning, the allocation of sufficient time, and the scheduling of the VR sessions in the two available VR rooms with stationary VR equipment. Thus, the care staff could not choose a more favorable day, or time of day, for each PwD to experience VR. Nevertheless, they were always compliant with the PwD’s mood in terms of their willingness and receptivity to experience VR, which could vary between the different scheduled VR sessions.
The difficulties that the care staff encountered included the PwD’s occasional refusals to go to the VR rooms, or cases in which they went along but quickly lost interest and wanted to return to the care unit after a short time. These refusals and moments of disinterest were assessed to be a result of the PwD’s worry, restlessness, agitation, and apathy or boredom with the films. As these BPSD usually built up during the day, a more suitable time for VR sessions would have been before lunch to avoid the build-up. Care staff considered the PwD’s stillness before the VR sessions to be a prerequisite to be able to enjoy the VR. The care staff became more familiar with the VR sessions as the intervention moved forward, and they understood the importance of taking a break between each film, taking off the PwD’s glasses, and talking about what had just been seen. A perfect fit of the glasses was important for the PwD to get a clear and sharp picture, whereas another difficulty was the uncertainty about whether the PwD had access to this quality of the visualization.
Owing to the meticulous staff planning, support from the management, allocation of sufficient time, and effective scheduling of the VR sessions, the study did not interfere with any routines in the care staff’s daily work, why using VR was regarded as both feasible and useful in the care for PwD. The feasibility was facilitated as the care staff shared joint responsibility for the PwD. During the study, when there were queries or concerns, the care staff members supported each other. Furthermore, all care staff were positive toward using VR in the future as part of an ordinary day. They suggested the use of mobile VR equipment so that more PwD could watch the films in the tranquility in their own rooms or in the care unit, as many PwD were reluctant to cross these physical boundaries. As one care staff member pointed out, “… the world is simply too big for them, and it frightens them.” Care staff stated that their selection of eligible persons for this study included those who were able to leave the care unit and comfortably walk to the VR room, thus excluding those who were in a more severe stage of their dementia. A mobile unit inside the care unit would therefore allow these PwD to experience VR while in the security of their familiar surroundings in the care unit. Furthermore, care staff considered that a mobile unit would provide the care staff and PwD with a greater choice of when to experience VR depending on the PwD’s mood, BPSD, and request. For some PwD, their worry, restlessness, agitation, or apathy hindered them from leaving the care unit, while these BPSD may have been mitigated (or PwD could have been distracted from them) if there had been an opportunity to experience VR in the care unit prior to lunch before the BPSD had built up too high. Care staff recommended that more films be produced, including those that reminded the PwD about their child- and adulthood, films with more “action”, and films where the PwD virtually moved their body forward instead of being required to stand in one place and look around.
Discussion
Considerations of the Results
The aims of this SCR study were to evaluate the individual use of VR in relation to PwD’s BPSD, quality of life, and medication use during an eight-week long intervention period, and to describe the care staff’s experiences of the usability and feasibility of VRin their care for PwD in a nursing home setting. In summary, no major differences in the quantitative data in terms of BPSD, quality of life, or medication use were found. However, as the frequency and severity of BPSD were relatively low during the pre-intervention, there was little room left for a decrease in BPSD as an outcome of the intervention. This was also the case concerning medication use. The qualitative data showed that the use of VR provided the PwD with short-term enjoyment, heightened energy and alertness, experiences of reminiscence and generated new topics of conversation. The care staff considered the use of VR to be both useful and feasible.
Instead of considering the data collection as sequentially explanatory (where quantitative data has the priority), data collection should be viewed as a concurrent case triangulation where both quantitative and qualitative data are assigned equal weights 45. According to the qualitative data, i.e., the care staff’s notes written in conjunction with each VR session and in group interviews; the VR sessions had an overall positive effect on PwD’s well-being. However, this effect was inconsistent with the quantitative data, i.e., the care staff’s assessments of PwD’s BPSD and quality of life as exhibiting no major differences in improvement, although a stabilizing trend during intervention was found for some PwD.
The qualitative data revealed that the VR increased nearly all PwD’s experience of joy and, for some, also their energy and alertness. In nearly all PwD, the VR triggered an experience of reminiscence, which, aside from being beneficial in prompting new topics of conversation between them and their care staff, was also valuable for augmenting a sense of self. The declines in memory among PwD have been argued to result in a “loss of self” 30. The memories invoked by the VR session and spoken of for the first time with care staff, must therefore be considered as valuable insofar as they could help augment the sense of self. VR allowed the PwD to temporarily step outside of their closed physical environment of the long-term care facility and be transported into an, albeit virtual, world of reminiscence. When PwD are institutionalized, their lives are disrupted, and their continuity is broken 46. Thus, VR sessions could provide them with a “memory sanctuary” to maintain this otherwise disrupted continuity of self. Therefore, it would be misleading to evaluate the intervention for each PwD only in terms of quantitative assessments performed biweekly, as it would disregard the PwD’s immediate experiences of intensified joy, energy, and reminiscence.
There is no one-size-fits-all care for PwD. Even when PwD exhibit similar BPSD, individual differences supersede the diagnoses, which might explain why the use of VR had an overall positive effect on certain PwD and not on others. Moreover, several challenges had to be dealt with during the intervention phase owing to the cognitive impairment of the PwD, as discussed by Lepore, Shuman, Wiener, and Gould 47. The importance of executing the intervention protocol was sometimes not understood by the PwD. In order not to violate the PwD’s personal integrity and to avoid raising ethical issues, the care staff had to comply with the PwD’s behavior and wait until the next scheduled time for a VR session. It would be beneficial in future studies to use mobile VR units for several reasons, including the alleviation of PwD’s worry and restlessness, and the care staff’s work load would presumably decrease if not having to leave the care unit to move to a stationary VR equipped room.
The present study did not explore the possible effects that the progression of dementia might have exerted on the outcomes of the intervention. As the severity of the cognitive decline became a limitation in the study by Siriaraya and Ang 30 when PwD’s visual and audio incapabilities hindered their immersion and focus in the VR experience, we can assume a similar limitation in our study if the care staff had not limited the participation to only those PwD who were expected to have the capability to complete the study, i.e., those with moderate progression of dementia.
Methodological Considerations
Several key issues of concern are associated with involving PwD as research participants, including recruitment, research ethics, the processes of obtaining informed consent and assent/dissent to participate in the research, communication challenges, and the reliability of the data 43. Since obtaining signed informed consent from the PwD was not always possible, the assent/dissent process was carefully considered throughout the study. To uphold the ethical principles, participation assent was obtained from the PwD at the beginning of every VR session as the mood and willingness to experience VR could vary from day to day. In all cases, the next of kin (e.g., spouse or children) or the trustees were asked if they objected to the PwD’s participation in the study, as it was questionable whether the PwD could communicate relatively consistently, understand the basic information regarding the choices, evaluate the implications of the different choices, and rationally comprehend the risks and benefits associated with the different options offered 48, 49. Since these capacities fluctuated over time and given that different decisions required different levels of capacity, a diagnosis of dementia or even a specific score on a cognitive test were not the only criteria for determining decision-making capacity 49.
Data evaluation in an SCR study focuses on whether the intervention can be identified as the cause for a change in the data measurements. A limitation in the present study was the limited number of data points collected during the intervention and post-intervention, which restricted the number of choices of data evaluation methods for the researchers. The available methods of data evaluation other than visual analysis, such as time series, interrupted time series, and percentage of all non-overlapping data (PAND), could have generated further reliable results, although these are not recommended for short, single-baseline SCR studies such as the present study 50. Visual inspection has been and continues to be the dominant and most reliable method for data evaluation in SCR studies 32, 42, which is why it was selected for the present study. Nonetheless, whether it was the intervention itself or other factors that influenced the changes remains unknown, especially as BPSD and quality of life were assessed only every other week during the intervention, meaning that several days could have passed between the VR session and the assessment. Had the assessments of BPSD and quality of life been carried out immediately adjacent to each VR session, or during the same day at the latest, we can assume that there would have been larger and more positive changes in BPSD and quality of life. In other words, the quantitative results would have been more consistent with the qualitative results.
Furthermore, since the exclusive presence and attention of one care staff member was assigned to each PwD for an hour, the Hawthorne effect could emerge as another limitation 51. This effect implies that the participants in a research study may change their behavior simply due to the extra attention received, irrespective of any experimental manipulation. Since no control was applied for this effect in the present study, it might have influenced the PwD’s BPSD, quality of life, and intensified joy, energy, alertness, and experience of reminiscence reported by the care staff.
SCR studies in clinical settings present several challenges for the researchers. The additional dimension of participants with cognitive impairments requires thoughtful attention from the researchers. It is possible to anticipate certain problems, such as the progression of dementia, employee turnover, and disturbances in the surroundings, but not others such as PwD’s lack of cooperation with research expressed through indications of frustration, discomfort, unhappiness, or passivity 47.
The present study was conducted in only one nursing home, and it is therefore not possible to generalize the results, although the results could be credible if the readers recognize the descriptions as comparable to their own experiences 52. Accordingly, the results may be transferable to other comparable situations and contexts.
Conclusions
The obtained data from the present study suggest that the use of VR provided short-term enjoyment, heightened energy and alertness, and experiences of reminiscence. These experiences were, however, inconsistent with the assessments of PwD’s BPSD and quality of life. There is no one-size-fits-all care for PwD. Even though PwD may exhibit similar BPSD, individual differences supersede the symptoms and diagnoses, which might explain why the use of VR had an overall positive effect on certain PwD but not on others. The inconsistency between qualitative and quantitative data in combination with PwD’s individual differences highlight the importance of care staff and their managers acquiring knowledge of available welfare technology and having the courage to promote, test, and systematically evaluate possible effects (or non-effects or non-suitability) of welfare technology among PwD. Despite these limitations, the care staff in this study considered the use of VR to be useful and feasible in their care for PwD, and VR may therefore serve as a complement to the non-pharmacological management techniques in the care of PwD in nursing homes.
Additional Materials
The data material generated during the current study is available from the corresponding author upon request.
Author Contribution
Christine Gustafsson designed and planned the study. Annelie K. Gusdal planned the study, implemented the intervention, and collected and analyzed the data. Annelie K. Gusdal wrote the major part of the manuscript in critical discussion with Christine Gustafsson. Both authors have approved of the final version submitted to Journal of Patient Care and Practices.
Acknowledgments
We wish to express our sincere gratitude to the participants who shared their experiences and perceptions so generously with us. We also thank Eskilstuna Municipality and Atea AB Sweden for professional collaborations.
Funding
This study was made possible through collaboration between the Department of Care and Support Management at Eskilstuna Municipality, Måsta Äng Academic Nursing Home, and the School of Health, Care, and Social Welfare at Mälardalen University. The company Atea AB Sweden made the study possible by leasing their VR equipment to Måsta Äng Academic Nursing Home.
List of Acronyms
BPSD - Behavioral and Psychological Symptoms of Dementia
NPI-NH - The Neuropsychiatric Inventory – Nursing Home
PwD - People (or Person/s) with Dementia
QUALID - Quality of Life in Late-Stage Dementia
SCR - Single-case Research
VR - Virtual Reality
References
- 1. (2020) World Health Organization. Fact sheet: Dementia. https://www.who.int/news-room/fact-sheets/detail/dementia;. , Accessed 6.
- 2.Cerejeira J, Lagarto L, Mukaetova-Ladinska E B. (2012) Behavioral and psychological symptoms of dementia. , Front Neurol 7(3), 1-23.
- 3.Kales H C, Gitlin L N, Lyketsos C G. (2015) Assessment and management of behavioral and psychological symptoms of dementia. BMJ.350:h369. Doi: 10.1136/bmj.h369 .
- 4.Toot S, Swinson T, Devine M, Challis D, Orrell M. (2017) Causes of nursing home placement for older people with dementia: a systematic review and meta-analysis. , Int Psychogeriatr 29(2), 195-208.
- 5.Fraser L A, Liu K, Naylor K L. (2015) Falls and fractures with atypical antipsychotic medication use: A population-based cohort study. , JAMA Intern Med 175(3), 450-452.
- 6.Wang P S, Schneeweiss S, Avorn J. (2005) Risk of death in elderly users of conventional vs. atypical antipsychotic medications. , N Engl J Med 353(22), 2335-2341.
- 7.Abraha I, Rimland J M, Trotta F M. (2017) Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop series. , BMJ 7(3), 012759-10.
- 8.Dyer S M, Harrison S L, Laver K, Whitehead C, Crotty M. (2018) An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. , Int Psychogeriatr.: 30(3), 295-309.
- 9.Cohen-Mansfield J, Thein K, Marx M S, Dakheel-Ali M, Freedman L. (2012) Efficacy of nonpharmacologic interventions for agitation in advanced dementia: A randomized, placebo-controlled trial. , J Clin 73(9), 1255-1261.
- 10.Legere L E, McNeill S, Schindel Martin L, Acorn M, An D. (2018) Nonpharmacological approaches for behavioural and psychological symptoms of dementia in older adults: A systematic review of reviews. , J Clin 27-7.
- 11.McDermott O, Charlesworth G, Hogervorst E. (2019) Psychosocial interventions for people with dementia: a synthesis of systematic reviews. , Aging Ment Health 23(4), 393-403.
- 12.Orgeta V, Qazi A, Spector A, Orrell M. (2015) Psychological treatments for depression and anxiety in dementia and mild cognitive impairment: Systematic review and meta-analysis. , Br J 207(4), 293-298.
- 13.Tsoi K, Chan J, Ng Y M, Lee M, Kwok T et al. (2018) Receptive music therapy is more effective than interactive music therapy to relieve behavioral and psychological symptoms of dementia: A systematic review and meta-analysis. , J Am Med Dir 19(7), 568-576.
- 14.JT van der Steen, Smaling H J, JC van der Wouden, Bruinsma M S, Scholten R J et al. (2018) Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev.;. 7(7).
- 15.Miller H L, Bugnariu N L. (2016) Level of immersion in virtual environments impacts the ability to assess and teach social skills in autism spectrum disorder. , Cyberpsychol Behav Soc 19(4), 246-256.
- 16.Cogné M, Taillade M, N'Kaoua B. (2017) The contribution of virtual reality to the diagnosis of spatial navigation disorders and to the study of the role of navigational aids: A systematic literature review. Ann Phys Rehabil Med.;60(3):. 164-176.
- 17.Coyle H, Traynor V, Solowij N. (2015) Computerized and virtual reality cognitive training for individuals at high risk of cognitive decline: systematic review of the literature. , Am J Geriatr Psychiatry 23(4), 335-359.
- 18.Dermody G, Whitehead L, Wilson G, Glass C. (2020) The role of virtual reality in improving health outcomes for community-dwelling older adults: Systematic review. , J Med Internet 22(6).
- 19.Hwang J, Lee S. (2017) The effect of virtual reality program on the cognitive function and balance of the people with mild cognitive impairment. , J Phys Ther Sci 29(8), 1283-1286.
- 20.Maggio M G, Maresca G, R De Luca.The growing use of virtual reality in cognitive rehabilitation: Fact, fake or vision? A scoping review. , J Natl Med Assoc 111(4), 457-463.
- 21.Manera V, Chapoulie E, Bourgeois J. (2016) A feasibility study with image-based rendered virtual reality in patients with mild cognitive impairment and dementia. , PLoS 11(3), 10-1371.
- 22.Moreno A, Wall K, Thangavelu K, Craven L, Ward E et al. (2019) A systematic review of the use of virtual reality and its effects on cognition in individuals with neurocognitive disorders. , Alzheimers Dement (N Y).; 5, 834-850.
- 23.Mrakic-Sposta S, Di Santo SG, Franchini F. (2018) Effects of combined physical and cognitive virtual reality-based training on cognitive impairment and oxidative stress in MCI patients: A pilot study. , Front Aging Neurosci 10, 282.
- 24.Smith S A. (2019) Virtual reality in episodic memory research: A review. Psychon Bull Rev. 26(4), 1213-1237.
- 25.Zucchella C, Sinforiani E, Tamburin S. (2018) The multidisciplinary approach to Alzheimer’s disease and dementia. A narrative review of non-pharmacological treatment. , Front Neurol 9, 1058.
- 26.Park M J, Kim D J, Lee U, Na E J, Jeon H J. (2019) A literature overview of virtual reality (VR) in treatment of psychiatric disorders: Recent advances and limitations. Front Psychiatry.;10: 505. Doi: 10.3389/fpsyt.2019.00505
- 27.Ferguson C, Shade M Y, Blaskewicz Boron J, Lyden E, Manley N A. (2020) Virtual reality for therapeutic recreation in dementia hospice care: A feasibility study. , Am J Hosp Palliat Care.; 24, 1-7.
- 28.Moyle W, Jones C, Dwan T, Petrovich T. (2018) Effectiveness of a virtual reality forest on people with dementia: A mixed methods pilot study. , Gerontologist 58(3), 478-487.
- 29.Reynolds L, Rodiek S, Lininger M, McCulley A. (2018) Can a virtual nature experience reduce anxiety and agitation in people with dementia?. , J Hous Elderly.; 32(2), 176-193.
- 30.Siriaraya P, Ang C S. (2014) Recreating living experiences from past memories through virtual worlds for people with dementia. The SIGCHI Conference on Human Factors in Computing Systems. CHI Conference on Human Factors in Computer Systems; , New York: 3977-3986.
- 31.Gusdal A K, Gustafsson C. (2020) Using a Rocking Chair in the Care of People with Dementia: A Single Case Research Study. , OBM Geriatrics 4(2), 10-21926.
- 32.Kazdin A E. (2011) . Single-Case Research Designs: Methods for Clinical and Applied Settings. 2nd ed , New York: OxfordUniversityPress .
- 33.Lobo M A, Moeyaert M, Baraldi Cunha A, Babik I. (2017) Single-case design, analysis, and quality assessment for intervention research. , J Neurol Phys 41(3), 187-197.
- 34.RL. (2016) Considerations in writing about single-case experimental design studies. , Cogn Behav Neurol 29(4), 169-173.
- 35.Samsung. (2020) Samsung Gear VR -. SM-R323 - headset. https://www.samsung.com/us/business/support/owners/product/gear-vr-sm-r323/; 2020 Accessed 6 .
- 36.D'Cunha N M, Nguyen D, Naumovski N. (2019) A mini-review of virtual reality-based interventions to promote well-being for people living with dementia and mild cognitive impairment. , Gerontology 65(4), 430-440.
- 37.Cummings J L. (1997) The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology.;48(5-6): 10-16. Doi: 10.1212/wnl.48.5_suppl_6.10s
- 38.Melander C, Sävenstedt S, Olsson M, Wälivaara B M. (2018) Assessing BPSD with the support of the NPI-NH: a discourse analysis of clinical reasoning. , Int Psychogeriatr 30(4), 581-589.
- 39.Falk H, Persson L O, Wijk H. (2007) A psychometric evaluation of a Swedish version of the Quality of Life in Late-Stage Dementia (QUALID) scale. , Int 19(6), 1040-1050.
- 40.Weiner M F, Martin-Cook K, Svetlik D A, Saine K, Foster B et al. (2000) The quality of life in late-stage dementia (QUALID) scale. , J Am Med Dir 1(3), 114-116.
- 41.Hsieh H F, Shannon S E. (2005) Three approaches to qualitative content analysis. , Qual Health Res 15(9), 1277-1288.
- 42.Lane J D, Gast D L. (2014) Visual analysis in single case experimental design studies: Brief review and guidelines. Neuropsychol Rehabil.;24(3-4):. 445-463.
- 43. (2018) World Medical Association. Declaration of Helsinki: Ethical principles for medical research involving human subjects. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/;. , Accessed 6.
- 44.ICMJE International. (2019) Committee of Medical Journal Editors. Recommendations for the Protection of Research Participants. http://www.icmje.org/recommendations/browse/roles-andresponsibilities/protection-of-research-participants.html;. , Accessed 6.
- 45.Creswell J W, Plano Clark VL. (2017) . Designing and Conducting Mixed Methods Research. 3rd ed. Thousand Oaks, CA:Sage Publications .
- 46.Lin Y C, Dai Y T, Hwang S L. (2003) The effect of reminiscence on the elderly population: A systematic review. Public Health Nurs. 20(4), 297-306.
- 47.Lepore M, Shuman S B, Wiener J M, Gould E. (2017) Challenges in involving people with dementia as study participants in research on care and services. Research summit on dementia care. Building evidence for services and supports. https://aspe.hhs.gov/basic-report/challenges-involving-people-dementia-study-participants-research-care-and-services;. , Accessed 9.
- 48.Karel M J, Gurrera R J, Hicken B, Moye J. (2010) Reasoning in the capacity to make medical decisions: The consideration of values. , J Clin Ethics 21(1), 58-71.
- 49.Woods B, Pratt R. (2005) Awareness in dementia: Ethical and legal issues in relation to people with dementia. Aging Ment Health. 9(5), 423-429.

