Isotretinoin-Induced Facial Hyperpigmentation: Idiosyncratic Reaction?
Abstract
Isotretinoin is notorious for having a myriad of mucocutaneous side effects including cheilitis, xerodermia, facial erythema, pruritis, hair thinning, and brittle nails, among others. Although photosensitivity is considered to be one of the side effects of oral isotretinoin therapy, cutaneous hyperpigmentation has not, to the best of our knowledge, yet been reported as a side effect. This report presents a case of striking facial hyperpigmentation in a patient on oral isotretinoin.
Author Contributions
Academic Editor: Kavitha Reddy, Boston University School of Medicine, MA 02118, United States.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2015 Ali Halawi, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Case Report
Isotretinoin is notorious for having a myriad of side effects involving several organ systems. Cheilitis is often listed as the most significant mucocutaneous adverse reaction.1, 2, 3 Other ones such as xerodermia, facial erythema, pruritis, hair thinning, brittle nails, and epistaxis are to name but a few.2, 3 Moreover, polymorphous erythema, pityriasis rosea-like eruptions, and urticaria are examples of uncommon allergic reactions that have been reported.1 Other side effects include pyogenic granulomas,4, 5 pyoderma gangrenosum,6 and acquired port wine stain.7 A single case of a patient who suffered severe hyperpigmentation of several body parts while on retinoid-PUVA (re-PUVA) treatment for generalized lichen planus has also been reported. Granted that PUVA therapy is indeed associated with transient pigmentary change, the true identity of the culprit remained unclear in that combination.8 However, oral isotretinoin has not yet been shown to cause cutaneous hyperpigmentation to the best of our knowledge. This report presents a case of striking facial hyperpigmentation in a patient on oral isotretinoin.
A 30-year-old man presented with a 4-month history of increased facial pigmentation. The patient reported that this had occurred 3 months after being started on oral isotretinoin (40 mg daily) for the treatment of acne vulgaris. He was otherwise healthy and not on any other drug therapy. In addition, he denied using any facial creams at the time when the problem had started. Moreover, he denied family history of similar condition or photodermatosis. On examination, the patient had well-demarcated hyperpigmented patches and plaques on an erythematous purpuric background (Figure 1). The changes were mainly observed on sun exposed surfaces. A punch biopsy was done and revealed dermal lymphohistiocytic infiltrates with scattered eosinophils, extravasated erythrocytes, and prominent hemosiderin deposition highlighted by iron stain (Figure 2). Fontana-Masson stain revealed no increase in melanin in the dermis or epidermis and immunohistochemical staining using MART-1 revealed normal melanocyte number at the basal cell layer of the epidermis.
Figure 1.(a) and (b) Increased facial pigmentation manifesting as well-demarcated hyperpigmented patches and plaques on an erythematous purpuric background predominantly in sun-exposed areas.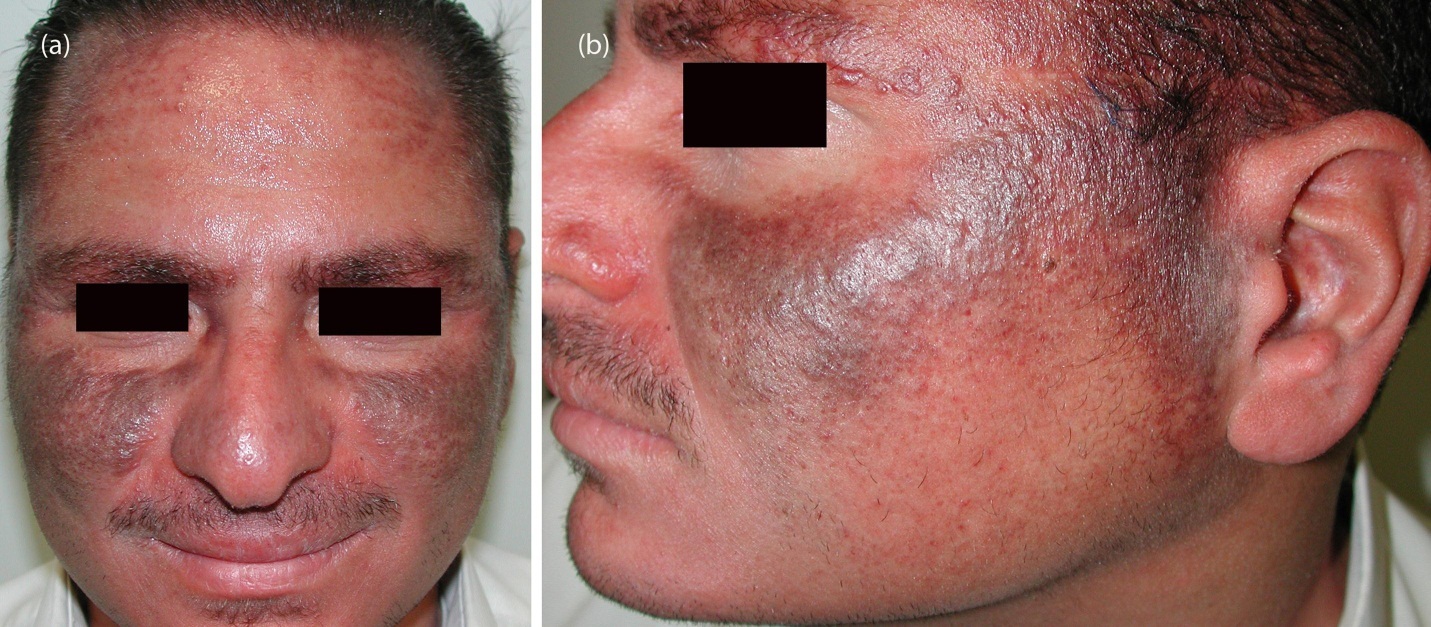
Figure 2.Histology revealed dermal lymphocytic infiltrates with scattered eosinophils, extravasated erythrocytes, and hemosiderin deposition (original magnification, 20). Inset: Perl’s stain highlights hemosidrin depostion (original magnification, 40).
By increasing epidermal turn-over and thinning the stratum corneum, retinoids, including isotretinoin, may rarely be associated with photosensitivity.3, 9 This light sensitivity may cause macular erythema often manifesting in the form of facial irritant dermatitis which is often observed in patients undergoing treatment during spring or summer.2 This could then lead to post-inflammatory hyperpigmentation (PIH), which is a reactive hypermelanosis that occurs secondary to a variety of inflammatory processes including endogenous, such as acne vulgaris, or exogenous, such as phototoxic reactions.10 However, some studies conducted on subjects taking isotretinoin revealed within-normal phototesting results and that the retinoid concentrations necessary to induce significant phototoxicity were rather elevated compared to the usual dosages. This might in turn be the reason for which not all patients on the drug exhibit abnormal photosensitivity.9 Furthermore, retinoids have been used, at concentrations of 0.01% to 0.1%, to successfully treat PIH.10 Their topical application enhances epidermal turn-over and the shedding of melanin, and concomitantly declines melanosome transfer. Moreover, retinoic acid appears to prevent the induction of melanogenesis by ultraviolet-B radiation (UVB).11 Indeed, hypopigmentation has been observed in patients on isotretinoin therapy.3 A patient with a 10-year history of acne vulgaris had used oxytetracycline and minocycline followed by topical clindamycin and benzoyl peroxide. She suffered from hyperpigmentation affecting her cheeks, chin, and forehead which resolved upon being started in isotretinoin 60 mg once daily.12 Paradoxically, our patient developed hyperpigmentation in the same areas while on oral isotretinoin as opposed to the resolution observed in the case just mentioned. This brings us back to the patient who sustained hyperpigmentation while on re-PUVA. The severe reaction could have been due to the use of a combination of two photosensitizers, psoralens and isotretinoin.8 Although PIH would also be considered in the differential diagnosis of our patient, the fact that the onset of hyperpigmentation occurred 3 months after initiating the drug and being mainly caused by hemosidrin deposition suggests that the administration of the drug itself may have been implicated somehow, possibly through an idiosyncratic reaction.
Hemosiderin deposits are usually observed in types I and II of minocycline-induced cutaneous hyperpigmentation, while type III does not involve iron deposition. The underlying mechanisms for the different types of minocycline-induced hyperpigmentation vary.13 One postulation is that minocycline and its derivatives form complexes with iron that deposit in the skin.14 Another one presumes the formation of a hypersensitivity reaction to antigens.15 Genetic factors, predisposing preexisting actinic damage, sunlight, and concomitant medications seem to be implicated too.16 Our patient was not taking any other medications, and the negative clinical family history may make the contribution of genetic factors unlikely. Still, the findings in our patient may suggest a similar mechanism by which type I minocycline hyperpigmentation occurs. Interestingly, a case of isotretinoin-induced pigmented purpuric dermatosis (PPD) on the lower extremities of a young adult woman has recently been reported. The clinical and pathological findings in our case were greatly similar.16
In summary, drug-induced photosensitization could be a possibility but is unlikely to have been solely responsible for the dramatic reaction our patient experienced taking into consideration previous reports. More importantly, the presence of hemosiderin deposits parallels a recently reported case of isotretinoin-induced PPD and what happens in some types of minocycline-induced reactions which may reflect an iron-chelating function of isotretinoin or its metabolites. In our case, we believe isotretinoin was the most likely causative agent because the lesions began after isotretinoin initiation and were slowly resolving after its termination. Based on this, it is important to consider isotretinoin as potential causative agent of drug-induced hyperpigmentation.
References
- 1.Brito Mde F, Sant'Anna I P, Galindo J C, Rosendo L H, Santos J B. (2010) Evaluation of clinical adverse effects and laboratory alterations in patients with acne vulgaris treated with oral isotretinoin. An Bras Dermatol. 85, 331-337.
- 2.Kaymak Y, Ilter N. (2006) The results and side effects of systemic isotretinoin treatment in 100 patients with acne vulgaris. Dermatol Nurs. 18, 576-580.
- 3.Lowenstein E B, Lowenstein E J. (2011) Isotretinoin systemic therapy and the shadow cast upon dermatology's downtrodden hero. Clin Dermatol. 29, 652-661.
- 4.Türel A, Oztürkcan S, Sahin M T, Türkdogan P. (2003) A rare side-effect of systemic isotretinoin treatment: pyogenic granuloma. , J Eur Acad Dermatol Venereol 17, 609-611.
- 5.Armstrong K, Weinstein M. (2011) Pyogenic granulomas during isotretinoin therapy. , J Dermatol Case Rep 5, 5-7.
- 6.Freiman A, Brassard A. (2006) Pyoderma gangrenosum associated with isotretinoin therapy. , J Am Acad Dermatol 55, 107-108.
- 7.Hoque S, Holden C. (2005) Acquired port wine stain following oral isotretinoin. Clin Exp Dermatol. 5, 587-588.
- 8.Carlin C S, Florell S R, Krueger G G. (2002) Induction of dramatic hyperpigmentation in a patient with generalized lichen planus treated with re-PUVA. , J Cutan Med Surg 6, 125-127.
- 9.Ferguson J, Johnson B E. (1986) Photosensitivity due to retinoids: clinical and laboratory studies. , Br J Dermatol 115, 275-283.
- 10.Callender V D, St Surin-Lord S, Davis E C, Maclin M. (2011) Postinflammatory hyperpigmentation: etiologic and therapeutic considerations. , Am J Clin Dermatol 12, 87-99.
- 12.Winhoven S M, Ahmed I, Owen C M, Lear J T. (2005) Postinflammatory hyperpigmentation in an Asian patient: a dramatic response to oral isotretinoin (13-cis-retinoic acid). , Br J Dermatol 152, 368-369.
- 13.Mouton R W, Jordaan H F, Schneider J W. (2004) A new type of minocycline-induced cutaneous hyperpigmentation. Clin Exp Dermatol. 29, 8-14.
Cited by (2)
This article has been cited by 2 scholarly works according to:
Citing Articles:
Awadh M. Alamri, Dhaii Alzahrani, Ghadi Alharbi, Rami Jan, Lulu Abdullah Alsubaie et al. - Clinical, Cosmetic and Investigational Dermatology (2025) Semantic Scholar
Clinical Cosmetic and Investigational Dermatology (2025) OpenAlex
Clinical, Cosmetic and Investigational Dermatology (2025) Crossref
